Glutamic Acid Decarboxylase Autoantibodies Role in Reclassifying Diabetes of Adulthood in Basrah
Abbas Ali Mansour1* [...] and Ali Hussein Ali Alhamza3
Abstract
Aim:
To determine the prevalence and phenotypic characteristics of diabetes subtypes based on glutamic acid decarboxylase autoantibodies (GADA) status in those newly presented diabetic to the Al-Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC) in Basrah, Southern Iraq.
Methods :
The study design is cross-sectional and includes adult diabetic patients if they are free of insulin treatment for at least 6 months from diagnosis and to be 30 years of age and over from the period of January 2013 to March 2013.
Results:
Of our diabetics with age 30 years and more, 26.4% were GADA-positive. The only significantly higher variables seen more among GADA-positive diabetes groups were normal weight and current insulin uses. GADA-positivity was not associated with gender, age, BMI, family history, smoking, hypertension, duration of diabetes, or specific HbA1c in the current study.
Conclusion:
A quarter of adults diabetic in Basrah were GADA positive. GADA positivity means more likely to be normal weight diabetics and currently on insulin use.
Introduction
Glutamicacid decarboxylase autoantibodies (GADA), also called 65kDa antibodies, is the most frequent form of autoantibodies in type 1 diabetic children and also occurs in some patients who initially present with adult-onset non-insulin requiring diabetes, also called latent adult-onset autoimmune diabetes (LADA) [1]. GADA is no longer only used in theory but are beginning to be used in clinical practice to reclassify type 2 diabetes mellitus [2].
LADA was introduced in 1994 to separate a GADA positive subgroup of adult patients initially diagnosed with type 2 diabetes [3]. Using this definition with the add-on criteria of no exogenous insulin during the first 6–12 months, the prevalence of LADA among unselected “type 2 diabetic patients” is variable, ranging between 25% in subjects less than 35 years and between 4 and 13% in subjects older than 35 years at diagnosis in diabetics of European origin [4].
On follow up researches, a progressive defect in insulin secretion was observed in 50–60% of LADA patients within 6–10 years [5], which led the World Health Organization (WHO) to include those patients in a category called a slowly progressing form of type 1 diabetes in the classification of diabetes [6].
LADA is clearly different from type 2 diabetes, in that LADA is associated with histocompatibility (HLA) genes, diabetes-associated autoantibodies, less insulin secretion, no need for insulin therapy initially after diagnosis, and less prevalence of metabolic syndrome [7]. And it’s may be considered as a slowly progressive form of autoimmune β-cell destruction, given that people with LADA have evidence of islet autoimmunity, namely circulating islet antibodies and type 1 diabetes susceptibility HLA class II alleles DQ2 and/or DQ8 [8]. A majority of adults with diabetes in the United Kingdom Prospective Diabetes Study (UKPDS), who had detectable GADA, required insulin treatment within 6 years of diagnosis [5].
A suggestion for diagnostic criteria for LADA as the age of 30 years or more at clinical presentation and not requiring insulin for > 6 months post-diagnosis might help with the definition of this disease [9], which represent a variable proportion (2–22%) [10]. In a large cohort of white European diabetics (n =3, 672) aged 25 –65 years in the UKPDS, the prevalence of LADA was 10% [5].
GADA persist in LADA for several years after diagnosis, which is in contrary to what observed in classical Type 1 diabetic patients [11]. LADA patients have a similar risk of complications and death to patients with clinically diagnosed type 2 diabetes without GADA, except for a lower prevalence and incidence of nephropathy [12]. There are suggestions that LADA phenotype is different from that of patients with GADA negative type 2 diabetes [13], with some features (including younger age, relative leanness and greater glycemia) that could influence the development of complications, at least theoretically. At diagnosis, patients with adult-onset autoimmune diabetes are usually non – insulin requiring and clinically indistinguishable from patients with type 2 diabetes though they tend to be younger and leaner. Only with screening for autoantibodies, especially GADA, can they be identified with certainty [7].
In the age limit, the Immunology of Diabetes Society had suggested an age limit of ≥30 to define LADA [14]. However, this is not always universal, as islet antibody-positive and slowly progressive diabetes has also been described in patients less than 30 years of age [15].
The aim of this study was to determine the prevalence and phenotypic characteristics of diabetes subtypes based on GADA status in those newly presented diabetic (regardless the duration of diabetes) to the Al-Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC) in Basrah, Southern Iraq.
Subjects, Materials and Methods
Setting
FDEMC is a tertiary referring center in Basrah Southern Iraq. The ethics committee in the Basrah College of Medicine approved the study.
Design
The study design is cross-sectional and includes adult diabetic patients if they are free of insulin treatment for at least 6 month from diagnosis and to be 30 years of age and over for the period of January 2013 to March 2013. Diabetes was designated according to standard criteria, and LADA was defined as patients aged at time of diagnosis 30 years or more with GADA-positive who did not require insulin treatment for at least 6 months after diagnosis [16]. Participants were classified according to the following definitions: type 1 diabetes, insulin-dependent <6 months from diagnosis; LADA, GADA-positive, age ≥ 30 years and insulin-independent ≥6 months from diagnosis; type 2 diabetes, GADA-negative and insulin-independent ≥6 months from diagnosis.
Exclusion criteria: Patients with incomplete data, current pregnancy, renal disease with a raised creatinine level.
All patients were given informed consent form. Data were collected on clinical characteristics (age, gender, symptoms, family history of diabetes, anthropometric features: height, weight, BMI, biological parameters like glycosylated hemoglobin (HbA1c), immunological markers (GADA).
Variables
Current smoking was defined as smoking all or part of a cigarette within the 30 days preceding the enrollment.
Family history of diabetes was defined as having diabetes in any of the following family members: parents, grandparents (either paternal or maternal), and siblings.
Height and weight were measured without shoes and heavy clothes. BMI was calculated as weight in kilograms divided by the square of height in meters.
Hypertension was defined as systolic blood pressure 140 mmHg or more and or diastolic blood pressure 90 mmHg or more on two occasions in seated patients for at least 5 minutes or history of hypertension and currently on drugs.
Biochemical tests
Blood (10mL) was collected for determination of biochemical parameters. HbA1c was determined by high-pressure liquid chromatography (HPLC) using D-10 Hemoglobin Testing System from Bio-Rad Laboratories, Inc., Hercules, CA 94547.
Antibody Measurement
Estimation of GADA.GADA were determined by GAD kit (Diametra, Italy). The kit was used for an in vitro qualitative ELISA test for detection of circulating autoantibodies against GAD antigens. (Sensitivity: 92,3%; Specificity: 98,6%).The intra-assay variability is ≤ 7.6%,and inter-assay variability is ≤8.2%. The upper normal limit for anti-GAD is 4 unit/ml. Subjects were considered positive for GADA if the value was 5 U/ml or higher.
Statistical Analysis
For continuous variables, the comparisons between GADA group and others were based on the t test as univariate analysis. Similarly, for categorical variables, the x2 test was used. Data were considered significant at P<0.05. Statistical analysis was performed using SPSS-15 statistical software.
Results
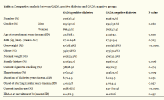
Total enrolled patients were 760 (Table 1). They were divided into two groups (GADA- positive diabetes and GADA- negative). GADA-positive diabetes constituted 26.4% of this cohort (57.2% men). Mean age of GADA- positive diabetes group was 40.8±8.1 years, which was not statistically different from that GADA-negative. The mean BMI was 27.1±24.8 kg / m2 with no significant difference from GADA-negative. Of those GADA-positive diabetes, 53.3% was having normal weight vs. 32.3% GADA-negative (P<0.0001). Family history was positive in 59.7% and current cigarette smoking was seen in 18.9% of GADA-positive patients, respectively, but none of these statistically different from GADA-negative. About 13.4% of GADA-positive were hypertensive, which is again not statistically different from those GADA-negative.
There was no difference between two groups in the duration of diabetes or onset of starting insulin, but 78.6% of GADA-positive were currently on insulin (P<0.0001). Again, presenting HbA1c not different between the two groups.
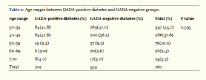
GADA-positive diabetes, according to age group is present in (Table 2). About 45.7% of the patients were in the age group 30-39 year. No significant difference in GADA positivity in all age groups (P value=0. 595).
Discussion
Of our diabetics with age 30 years and more, 26.4% were GADA-positive. The only significantly higher variables seen more among GADA-positive diabetes groups were normal weight and current insulin users in this study. GADA-positivity was not associated with gender, age, BMI, family history, smoking, hypertension, duration of diabetes, or specific HbA1c in the current study.
The family history among patients with LADA are conflicting among studies. Some people suggest that LADA patients are unlikely to have a family history of type 2 diabetes [17], while Carlsson et al indicate presence of family history as an important risk factor for the development of LADA [18].
The studies on LADA in the Middle East were scanty. We come across one study from Iran, where, among 500 patients with type 2 diabetes GADA positivity was reported in 14.2%. GADA positivity was more associated with 50–59 Years, but not associated with hypertension, family history of diabetes, and cigarette smoking [19].While in Saudi Arabia, of patients with type 2 DM, 8/99 patients were GADA positive [20]. Furthermore, in a small cohort from Turkey GADA-positive cases were seen in 31%among 54 initially diagnosed type 2 diabetic patients [21].
Different data reported from Africa, where the prevalence range 14%in Nigeria to 13.5% in Ghana to 7.3% in Tanzania [22-24].
Furthermore, in Asia, GADA were detected in 16.1 % of Chinese type 2 diabetic patients [25]. And the prevalence of GADA-positive diabetes cohort from three largest hospitals in Sri Lanka was 5.4% (n = 54; 95% CI 4.0 – 6.8). The prevalence of GADA positivity was much higher among those who were young and had a lower BMI compared with those who were older and more obese [26]. GADA positivity among men and women was 7. 4% and 4.0%, respectively (p = 0.028). Compared with those that tested negative for GADA, GADA-positive participants had been diagnosed at a younger age, were leaner, had a lower frequency of hypertension, presented.
European data are exemplified in LADA in South Wales study, were the predictors of associations with increasing levels of GADA: younger age at presentation, increasing IA-2 concentration, decreasing C-peptide concentration, presence of other autoimmune disorders, lower BMI and increasing HbAlc [27]. Factors not statistically significant included: symptom at presentation, family history of diabetes and family history of other autoimmune disorders. Multivariate analysis revealed that, out of the above, higher GADA levels were associated with higher IA-2, higher HbA1c, younger age and lower BMI. Ethnic background was not included in the analysis as 98.4%of the sample population were Caucasian [27].
Conclusion
A quarter of adults diabetic in Iraq are GADA positive. GADA positivity means more likely to be normal weight diabetics and currently on insulin use.
Acknowledgment
The authors would like to acknowledge all the medical staff of Al-Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Article information
Articles from International Journal of Clinical Endocrinology and Metabolism are provided here courtesy of Peertechz
References
- Leslie RD, Williams R, Pozzilli P (2006) Clinical review: Type 1 diabetes and latent autoimmune diabetes in adults: one end of the rainbow. J Clin Endocrinol Metab 91: 1654-1659.
- Törn C, Mueller PW, Schlosser M, Bonifacio E, Bingley PJ, et al. (2008) Diabetes Antibody Standardization Program: evaluation of assays for autoantibodies to glutamic acid decarboxylase and islet antigen-2. Diabetologia 51: 846-852.
- Zimmet PZ, Tuomi T, Mackay IR, Rowley MJ, Knowles W, Cohen M, et al. (1994) Latent autoimmune diabetes mellitus in adults (LADA): the role of antibodies to glutamic acid decarboxylase in diagnosis and prediction of insulin dependency. Diabet Med 11: 299-303.
- Buzzetti R , Di Pietro S, Giaccari A, Petrone A, Locatelli M, et al. (2007) Non Insulin Requiring Autoimmune Diabetes Study Group. High titer of autoantibodies to GAD identifies a specific phenotype of adult-onset autoimmune diabetes. Diabetes Care 30: 932-938.
- Turner R, Stratton I, Horton V, Manley S, Zimmet P, et al. (1997) UKPDS 25: autoantibodies to islet-cell cytoplasm and glutamic acid decarboxylase for prediction of insulin requirement in type 2 diabetes. UK Prospective Diabetes Study Group. Lancet 350: 1288-1293.
- Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15: 539-553.
- Hosszúfalusi N, Vatay A, Rajczy K, Prohászka Z, Pozsonyi E, et al. (2003) Similar genetic features and different islet cell autoantibody pattern of latent autoimmune diabetes in adults (LADA) compared with adult-onset type 1 diabetes with rapid progression. Diabetes Care 26: 452-457.
- Tuomi T, Carlsson A, Li H, Isomaa B, Miettinen A, et al. (1999) Clinical and genetic characteristics of type 2 diabetes with and without GAD antibodies. Diabetes 48: 150-157.
- Palmer JP, Hampe CS, Chiu H, Goel A, Brooks-Worrell BM (2005) Is latent autoimmune diabetes in adults distinct from type 1 diabetes or just type 1 diabetes at an older age? Diabetes 54: S62-57.
- van Deutekom AW, Heine RJ, Simsek S (2008) The islet autoantibody titres: their clinical relevance in latent autoimmune diabetes in adults (LADA) and the classification of diabetes mellitus. Diabet Med 25: 117-125.
- Hampe CS, Kockum I, Landin-Olsson M, Törn C, Ortqvist E, et al. (2002) GAD65 antibody epitope patterns of type 1.5 diabetic patients are consistent with slow-onset autoimmune diabetes. Diabetes Care 25: 1481-1482.
- Myhill P, Davis WA, Bruce DG, Mackay IR, Zimmet P, et al. (2008) Chronic complications and mortality in community-based patients with latent autoimmune diabetes in adults: the Fremantle Diabetes Study. Diabet Med 25: 1245-1250.
- Niskanen LK, Tuomi T, Karjalainen J, Groop LC, Uusitupa MI (1995) GAD antibodies in NIDDM. Ten-year follow-up from the diagnosis.Diabetes Care 18: 1557-1565.
- Hawa MI, Kolb H, Schloot N, Beyan H, Paschou SA, et al. (2013) Action LADA consortium. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: Action LADA 7.Diabetes Care 36: 908-913.
- Lohmann T, Nietzschmann U, Kiess W (2000) "Lady-like": is there a latent autoimmune diabetes in the young? Diabetes Care 23: 1707-1708.
- Leslie RD, Kolb H, Schloot NC, Buzzetti R, Mauricio D, et al. (2008) Diabetes classification: grey zones, sound and smoke: Action LADA 1.Diabetes Metab Res Rev 24: 511-519.
- Latent Autoimmune Diabetes in Adults. Accessed 2014 Jul 4 .Available from: http://www.isletsofhope.com.
- Carlsson S, Midthjell K, Grill V (2007) Influence of family history of diabetes on incidence and prevalence of latent autoimmune diabetes of the adult: results from the Nord-Trøndelag Health Study. Diabetes Care 30: 3040-3045.
- Hossein GM, Maryam S, Saeed E, Hamid N, Mahdieh M (2015)The prevalence of latent autoimmune diabetes in adults and its correlates in patients with type 2 diabetes in Kerman, Iran [2011]. Diabetes Metab Syndr 9: 104-107.
- Damanhouri LH, Dromey JA, Christie MR, Nasrat HA, Ardawi MS, et al. (2005) Autoantibodies to GAD and IA-2 in Saudi Arabian diabetic patients. Diabet Med 22: 448-452.
- Arikan E, Sabuncu T, Ozer EM, Hatemi H (2005) The clinical characteristics of latent autoimmune diabetes in adults and its relation with chronic complications inmetabolically poor controlled Turkish patients with Type 2 diabetes mellitus. J Diabetes Complications 19: 254-258.
- Adeleye OO , Ogbera AO, Fasanmade O, Ogunleye OO, Dada AO, et al. (2012) Latent Autoimmune Diabetes Mellitus in Adults (LADA) and it's characteristics in subset of Nigerians initially managed for type 2 diabetes. Int Arch Med 5: 23.
- Agyei Fempong MT, Titty FV, Owiredu WK, Eghan BA (2008) The prevalence of autoimmune diabetes among diabetes mellitus patients in Kumasi Ghana. Pak J Biol Sci 11: 2320-2325.
- Lutale JJ, Thordarson H, Holm PI, Eide GE, Vetvik K (2007) Islet cell autoantibodies in African patients with Type 1 and Type 2 diabetes in Dar es Salaam Tanzania: a cross sectional study. J Autoimmune Dis 4: 4.
- Thai AC, Ng WY, Loke KY, Lee WR, Lui KF, et al. (1997)Anti-GAD antibodies in Chinese patients with youth and adult-onset IDDM and NIDDM. Diabetologia 40: 1425-1430.
- Katulanda P, Shine B, Katulanda GW, Silva A, Asfir EL, et al. (2008) Diabetes mellitus among young adults in Sri Lanka--role of GAD antibodies in classification and treatment: the SriLanka Young Diabetes study. Diabetologia 51: 1368-1374.
- Davies H, Brophy S, Fielding A, Bingley P, Chandler M, et al. (2008) Latent autoimmune diabetes in adults (LADA) in South Wales: incidence and characterization. Diabet Med 25: 1354-1357.
 ,
Ammar Mohamd Saead Almomin2 and Ali Hussein Ali Alhamza3
,
Ammar Mohamd Saead Almomin2 and Ali Hussein Ali Alhamza3