An Analytical Study for Early Diagnosis and Treatment of Infants & Children Suffering From Congenital Hypothyroidism in China
Fuyong Jiao1* [...] and Fangting Liu1
Abstract
Objective: :
To study the clinical and laboratory characteristics of children suffering from congenital hypothyroidism in China.
Method:
455 cases of congenital hypothyroidism infants were collected from 5 articles were published in 4 china medical journals. Different screening methods were adopted, like enzyme immunoassay assay and filter paper dried blood biotin-avidin enzyme notation to test TSH, FT3、FT. All the collected children treated by oral thyroxin tablets for long period and regular follow-up was done. Clinical follow up for any signs of hypothyroidism and also detection of I.Q of those children.
Results:
Markedly effective group: IQ >70%, height, constipation, lethargy, abdominal distension, jaundice and other symptoms and signs were improved after treatment. Effective group: IQ: 30%-70%, height, constipation, lethargy, abdominal distension, jaundice and other symptoms and signs were improved after treatment. Poor effective group: 0-30% IQ, while other signs and symptoms not much improved. Laboratory testing revealed au thyroid along with oral treatment of thyroxin in regular time and dose.
Conclusion:
Congenital hypothyroidism is a preventable disease if early diagnosis and treatment was done.
Introduction
Thyroid hormones are of prime importance in human growth and development [1]. The critical period for the central nervous system to be dependent on thyroid hormone is known to extend from fetal life until at least the first two years after birth [2]. Congenital hypothyroidism (CH) is a common pediatric endocrine disease which results from decrease in thyroid hormone secretion, and it of any cause is difficult to be recognized in neonatal period because of normal gross appearance [3]. The term ‘congenital hypothyroidism’ was introduced more than 60 years ago when Radwin et al. first described children with hypothyroid-associated features of severe intellectual disability and growth retardation. Nowadays, this definition of congenital hypothyroidism has to be revisited, on account of the diagnosis of the disease is made according to biochemical measurement of TSH and thyroid hormone levels alone, before the onset of severe clinical symptoms [4]. In this report will analyze diagnosis and treatment results of 455 cases suffering from congenital hypothyroidism.
Patients and Methods
Patients: 455 cases
(215 boys and 240 girls). 55.2% of them are younger than 6 months; 7.9% of them range from 6 months to 2 years old; the rest of them are between 3 to 7 years old.
Methods
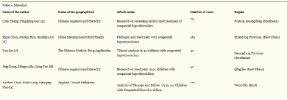
Collection of 455 cases of congenital hypothyroidism from 5 article in 4 China medical journals (Table 1); 163 patient were screened using enzyme immunoassay assay of (TSH), reference value <20uU/ml confirmed experiment by radioimmunoassay serum of TSH, FT4 and / or FT4 T3 content. while 73 cases of congenital hypothyroidism children were screened by experiment adopts enzyme immunoassay to test TSH, screening TSH>10m IU/L is positive, screening positive children will be recalled to screening center immediately, The one whose TSH 10-20mlL/L will be mining heel blood will be reviewed The one whose TSH>20mlU/L will be checked for FT3, FT4, TSH in extracted venous blood is to confirm diagnosis experiment. The confirm diagnosis experiment adopts immune analyzer which is produced by Switzerland Roche, whose reagent is specially used for thyroid hormone, and the detection method is electrochemical luminescence immunoassay.
In addition 169 cases of congenital hypothyroidism children were screened through TSH measurement using the filter paper dried blood films biotin - avidin enzymes of notation used kit produced by the United States Jinqiao diagnosis and referral of serum TSH, FT3, FT4 measured using radiation immunosorbent assay.
Results
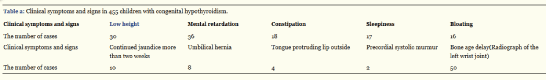
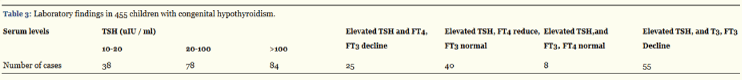
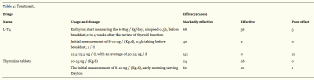
After analysis we can draw the following conclusions. Clinical symptoms and signs in 455 children with congenital hypothyroidism: Low height, Mental retardation, Constipation, Sleepiness, Bloating, Continued jaundice more than two weeks, Umbilical hernia, Tongue protruding lip outside, Precordial systolic murmur, Bone age delay (Radiograph of the left wrist joint) respectively 30, 36, 18, 17, 16, 10, 8, 4, 2, 50 (Table 2). Laboratory findings in 455 children with congenital hypothyroidism: 10-20, 20-100, >100 TSH (uIU / ml) respectively 38, 78, 84 cases. Elevated TSH and FT4, FT3 decline, Elevated TSH, FT4 reduce, FT3 normal, Elevated TSH, and FT3, FT4 normal, Elevated TSH, and T3, FT3Decline respectively 25, 40, 8, 55cases (Table 3). Markedly effective group: IQ >70%, height, constipation, lethargy, abdominal distension, jaundice and other symptoms and signs were improved after treatment. Effective group: IQ: 30%-70%, height, constipation, lethargy, abdominal distension, jaundice and other symptoms and signs were improved after treatment. Poor effective group: 0-30% IQ, while other signs and symptoms not much improved. Laboratory testing revealed au thyroid along with oral treatment of thyroxin in regular time and dose.
Discussion
Congenital hypothyroidism CH is mainly due to defect of thyroid tissue during embryonic development in form of dysplasia, absent or ectopic and thyroid hormone synthesis enzyme defects, resulting in inadequate secretion of thyroid hormone, which causes defect of body metabolism, growth retardation and mental retardation [10].
The term ‘congenital hypothyroidism’ is generally applied if the disorder is believed to have been present at or before birth. There is an accumulating evidence indicating that gene mutations may be a cause of increased incidence of congenital hypothyroidism [11]. Iodine deficiency is a major cause of hypothyroidism in children, which makes maternal and fetal thyroid uptake competitively limited iodide, so that maternal and neonatal thyroid hormone synthesis deficiency.
Children hypothyroidism is a common clinical endocrine disease. There are permanent CH and transient CH. The most frequent cause of permanent CH is thyroid dysgenesis, which results from defects in glandular formation during embryogenesis and the remaining due to defects in multiple pituitary hormone [12,13]. Whereas the underlying causes of transient CH functional impairment are less clear and may include maternal factors such as excessive or deficient iodine intake, anti-thyroid medication or presence of thyroid-stimulating hormone receptor (TSHR) antibodies during pregnancy heterozygous mutations in enzymes DUOX [12]. The incidence of permanent CH is higher than transient CH, while the TSH levels were significantly higher in patients with permanent CH than those with transient CH (p<0.004) [14].
The incidence of congenital hypothyroidism reported differently the incidence varies by geographic location and by ethnicity CH recorded prevalence’s between 1:2500 and 1:4000 [15,16]. However, newborn screening programmers have reported a rise in the incidence of CH to 1: 1400–1: 2800 infants, which attributed to the widespread screening strategies of thyroid function and to the diagnosis of milder cases of CH [17-19]. In recent years it is reported of 49.2/100000 in China [20].
The most frequent symptoms and signs of CH are mental retardation, poor growth, prolonged neonatal jaundice, hoarse cry, lethargy, slow movements, constipation, macroglossia, umbilical hernia, large fontanelle and dry skin. One prospective descriptive study reports from Razavi et al. [21]. Indicate that congenital hypothyroidism is associated with various forms of co-occurring congenital anomalies. However, most children with CH (> 95%) have little or no Clinical symptoms and detectable physical signs of the disease at birth because of the trans placental passage of maternal T4 and most affected children have some functioning thyroid tissue. As thyroid hormone has a half-life of 7 days, the maternal hormone is metabolized and excreted approximately 3-4 weeks after birth [13]. So the clinical signs of the hypothyroidism may gradually develop during infancy and childhood.
Thyroid hormone is critical for normal growth, skeletal and nervous system development of the fetus and newborn and CH is a primary cause of intellectual impairment for the first 2-3 years of life. Within six months after birth is the fastest period of brain development, if children with congenital hypothyroidism did not receive proper treatment within six months after birth or delay in time for treatment would cause irreversible mental retardation and poor growth. Early screening and early treatment play a vital role in congenital hypothyroidism. Infants who are diagnosed and treatment in the first three months have the best prognosis for optimal mental development [22].
CH in the neonatal period are diagnosed based on clinical manifestations only 6%, while in this stage blood biochemical changes have occurred, so it is very important for laboratory screening before clinical symptoms in children [23]. Analysis the above dates we can get these conclusions: in the 455cases,only 191 cases have clinical symptoms and signs, the percentage is 41.98%, but there are only 8 cases’ Laboratory results normal, the positive rate is up to97.56%,so the laboratory tests are very important in the diagnosis of congenital hypothyroidism. The definite diagnosis of CH depends on this so-called ‘confirmatory diagnosis’. Screening tests for CH that got abnormal results should be confirmed by quantitative measurement of venous TSH and total T4/free T4 [24]. TSH screening is more specific in the diagnosis of CH, T4 screening is shown to be more sensitive in detecting particularly those newborns with rare hypothalamic-pituitary-hypothyroidism, but it is less specific with a high frequency of false positives mainly in premature infants and low birth weight [25]. The high sensitivity of newborn screening tests for CH makes them an effective way to identify disease. However, screening for CH has certain degree of false-positive results [26]. In order to avoid misdiagnosis owing to a transient TSH surge or a sample error, serum measurement of TSH, T4 either total or free T4 and T3 is necessary before treatment can be initiated [4]. About 55%of the hypothyroid patients were detected within the first 6 months. Some scholars suggested that blood collection should be performed after 48 hours of birth to 4 days of life, in order to minimize the false positive high TSH on account of the physiological neonatal elevates TSH levels and causes dynamic T4 and T3 changes in the first 1 or 2 days after birth. In critically ill or preterm children, blood collection should be performed at 7 days of life. Meanwhile, some authors recommend repeating their screening test within 2 to 4 weeks of age on account of the immaturity of the hypothalamic-pituitary-thyroid axis in preterm infants [25,27]. CH is one of the most common preventable causes of mental retardation. Neonatal screening for thyroid function allow for the early detection and treatment of CH, thus preventing the mental retardation that results from the lack of thyroid hormone.
Thyroid disease and other diseases, timely and accurate diagnosis is essential. When the children’s symptoms, signs and laboratory test results do not coincide or are contradictory and atypical clinical manifestations, you cannot jump to conclusions, and need to double-check or other related testing. Meanwhile you must not categorically make a diagnosis based on a single blood thyroid hormones or auto antibodies numerical level, nor solely on the basis of radiological or pathological findings.
Oral administration of sodium L-T4 is the optimal choice for the treatment of CH. The American Academy of Pediatrics recommended the dose be 10-15 µg/kg.d, which should be initiated as soon as possible, ideally within the first 2 weeks of life, even if in the absence of clinical manifestations [27]. A findings suggested that, to a large extent, normal intellectual and motor development depend on a strategy of rapidly identifying and treating infants with CH using high-dose levothyroxine replacement [28]. Analysis the above dates we also get conclusions as follows, there are 332 cases treated with L-T4 in the 455 cases and the curative effect markedly is 78.01%, the effective is 17.47%,the invalid is only 4.52%,in these cases with an initial dose of 12.5-75.5μg, an average of 50.25μg per day, the curative effect markedly is highest, it tells us this dose having the best prognosis for congenital hypothyroidism; there are 123 cases treated with Thyroxin tablets, and the curative effect markedly is 69.92%, the effective is 29.27%,the invalid is only 0.81%, so in accordance with the curative effect markedly, congenital hypothyroidism is preferably treated with L-T4, treatment dose varies from person to person, mainly based on the level of serum TSH,FT4,FT3and thyroid function, condition. One study reported that over-treatment for CH during the first two years result in lowered cognitive outcomes at age 11. However, under-treatment, if not complicated by over-treatment, has a normal cognitive development scores regardless of ages. Fast TSH normalization at initial treatment result in above-normal development scores at age 1.8, but does not affect IQ at 11 y [29].
It is necessary for more frequent laboratory testing when there is poor compliance with the treatment or excessive treatment, according to the laboratory results can be to determine whether a change in the dosage. At the same time, avoiding for prolonged periods leading to craniosynostosis and changes in the child’s temperament. In a word, the goal of CH treatment is to ensure that the children have normal growth and psychomotor development as close as possible to their genetic potential.
Doctors should be familiar with a variety of pharmacological properties of thyroid hormone preparations, including medication that may arise after the efficacy and possible adverse reactions such as allergic reactions or toxicity. Based on children’s age, physical condition and other treatments while receiving, then you not only have to consider the medication in children with the disease severity, but also pay attention to children at this time whether able to withstand the dose of the drug, so that individualized dose. In case of hypothyroidism in children accompanied by heart, liver damage or other complications, the treatment of hypothyroidism in the same time, complications should be active and effective in the treatment and close observation. Doctors, determine for treatment should base on enough medicine evidence, obtain the consent of parents, and improve adherence to treatment in order to achieve the desired effect.
The newborn screening has been introduced for 40 years, although early detection and treatment has essentially rooted out severe intellectual impairment in the developed countries, one depressing question is that a few congenital hypothyroidism may still have mild neurodevelopment problems, such as movement slow, attention deficit and alterations in memory [30]. Some scholars think that are not related to the initial L-thyroxin dose or to the timing of treatment, but related to lower initial free T4 levels. Maternal hypothyroxinemia may be important in the long-term sequelae of congenital hypothyroidism, but further studies are needed to confirm [31].
Another noteworthy clinical question is whether these mild congenital hypothyroidism are transient or require permanent treatment. A retrospective studies from Olivieri et al. [32], they reviewed 1676 babies of congenital hypothyroidism, finding that 327(21.6%) patients with permanent CH had a mild TSH elevation (≤15.0 μU/mL) on screening. Specifically, 19.6% of these patients had thyroid dysgenesis. Meanwhile, it is noteworthy that the frequency of thyroid hypoplasia/hemiagenesis was similar in the group with TSH at screening of ≤15.0 μU/mL and in that with ≥15.0 μU/mL they suggested low the TSH cutoff in order to detect more cases of permanent CH. Similar results were got by Rabbiosi et al. [33]. Both studies used a standardized assessment of the need for ongoing treatment after 2–3 years old, overcoming a limitation of many prior studies. Their data support the conclusion that newborns with mild abnormalities on neonatal screening nonetheless have a significant risk of permanent congenital hypothyroidism that may become more severe in the future.
Besides, the training of family neurological rehabilitation is also critical for prognosis. Children with congenital hypothyroidism rehabilitation training can improve their communication, comprehension and social adaptability, and reduce the incidence of disability [34]. The regular neuropsychological follow-up in early treated congenital hypothyroidism, which is recommended to keep in mind the importance of the combination of neonatal endocrinological factors (in particular, pretreatment serum thyroxine) and sociocultural level (SCL) on the cognitive, motor and language development [35].
In the process of diagnosis and treatment of thyroid diseases, follow-up is a seemingly ordinary but very necessary clinical tool. Diagnostic is gradually clear for some children who are closely observed in the clinical follow-up. Calaciura et al. [36] studies have shown that elevated serum TSH values at screening examination but normal FT4 and either normal or slightly elevated TSH at the recall examination of neonatal will occur significantly higher probability for subclinical hypothyroidism in infancy and early childhood, so these newborn should closely follow-up. Clinical examination, including assessment of growth and development, ought to be inspected every few months during the first 3 years of life. The treatment effect of congenital hypothyroidism also depends on the follow-up: children receiving treatment under 3 months have monthly referral, 3 months to1 year old have every three months referral ,1 year old to 6 years and a half have a visit once a year. The main contents include referral serum TSH, T4, T3determination, growth and development, and intelligent detection.
Article information
Articles from International Journal of Clinical Endocrinology and Metabolism are provided here courtesy of Peertechz
References
- Gheissari A, Hashemipour M, Khosravi P (2012) Different aspects of kidney function in well-controlled congenital hypothyroidism. J Clin Res Pediatr Endocrinol 4:193-198.
- Zoeller Rt, Rouext J (2004) Timing of thyroid hormone action in the developing brain: clinical observations and experimental findings. J Neuroendocrionol 16: 804-818.
- Karamizadeh Z, Saneifard H, Amirhakimi G (2012) Evaluation of congenital hypothyroidism in fars province, iran.Iran J Pediatr 22: 107-112.
- Gruters A, Krude H (2012) Detection and treatment of congenital hypothyroidism[J].Nat Rev Endocrinol 8:104-113.
- Lixia Zhang, Pingming Gao (2012) Congenital hypothyroidism reduce disease screening results and treatment follow-up analysis of Chinese eugenics and Heredity 20: 62-63.
- Xigui Chen, Jinhua Han, Xianlian Jin (2005) Etiology and treatment of congenital hypothyroidism, China Maternal and Child Health 20: 1926-1928.
- Yun Lin (2009) clinical analysis of 42 cases of congenital hypothyroidism, China Modern Drug Application 3: 65-66.
- Jing Gong, Mingxu Shi, Tao Leng (2004) 50 cases of treatment of congenital hypothyroidism results analysis, Chinese Journal of Birth Health and Heredity12: 110-128.
- Xuelian Zhou, Huaqing Mao, Ru-Lai Yang (2007) congenital hypothyroidism 127 cases of Applied Clinical Pediatrics 22: 606-607.
- Cheng Zhu, Yujun Wu (2005) Growth retardation caused by hypothyroidism treatment. Chinese Journal of Pediatrics 20: 458-459.
- Srivastava D, Olson EN (2000) A genetic blueprint for cardiac development. Nature 407: 221-226.
- Bhavani N (2011) Transient congenital hypothyroidism Indian J Endocrinol Metab15: S117-120.
- Maciel LM, Kimura ET, Nogueira CR (2013) Congenital hypothyroidism: recommendations of the Thyroid Department of the Brazilian Society of Endocrinology and Metabolism. Arq Bras Endocrinol Metabo l57: 184-192.
- Bekhit OE, Yousef RM (2013) Permanent and transient congenital hypothyroidism in fayoum, egypt: a descriptive retrospective study. PLoS One 8: e68048.
- LaFranchi S (1999) Congenital hypothyroidism: etiologies, diagnosis, and management. Thyroid 9: 735-740.
- Hinton CF, Harris KB, Borgfeld L, Drummond-Borg M, Eaton R,et al. (2010) Trends in incidence rates of congenital hypothyroidism related to select demographic factors: data from the United States, California, Massachusetts, New York, and Texas.Pediatrics125: S37-47.
- Mitchell ML, Hsu HW, Sahai I (2011) The increased incidence of congenital hypothyroidism: fact or fancy? Clin Endocrinol (Oxf) 75: 806-810.
- Deladoey J, Ruel J, Giguere Y (2011) Is the incidence of congenital hypothyroidism really increasing? A 20-year retrospective population-based study in Quebec.J Clin Endocrinol Metab 96: 2422-2429.
- Albert BB, Cutfield WS, Webster D, Carll J, Derraik JG, et al. (2012) Etiology of increasing incidence of congenital hypothyroidism in New Zealand from 1993-2010. J Clin Endocrinol Metab 97: 3155-3160.
- Yanhua Xu, Yufeng Qin. Zhengyan Zhao (2009) Review of China newbore congenital hypothyroidism and phenylketonuria screening in 22 Years.Chinese Journal of Pediatrics 47: 18-22.
- Razavi Z, Yavarikia A, Torabian S (2012) Congenital anomalies in infant with congenital hypothyroidism. Oman Med J27: 364-367.
- Zhefeng Yuan, Yanfei Luo,Wu Yidong (2007) Congenital hypothyroidism and Han ethnic children thyrotropin receptor gene inactivating mutations. Chinese Journal of Pediatrics 45: 508-512.
- Jia Jin Zhou (2005) Congenital hypothyroidism clinical analysis of 25 cases. Medical Theory and Practice 18: 426.
- Zilka LJ, Lott JA, Baker LC (2008) Finding blunders in thyroid testing: experience in newborns. J Clin Lab Anal 22: 254-256.
- Clause M (2013) Newborn Screening for Congenital Hypothyroidism. J Pediatr Nurs 28: 603-608.
- Kwon C, Farrell PM (2000) The magnitude and challenge of false-positive newborn screening test results. Arch Pediatr Adolesc Med 154: 714-718.
- Rose SR, Brown RS, Foley T (2006) Update of newborn screening and therapy for congenital hypothyroidism. Pediatrics 117: 2290-2303.
- Albert BB, Heather N, Derraik JG (2013) Neurodevelopmental and body composition outcomes in children with congenital hypothyroidism treated with high-dose initial replacement and close monitoring. J Clin Endocrinol Metab 98: 3663-3670.
- Bongers-Schokking JJ, Resing WC, de Rijke YB, de Ridder MA, de Muinck Keizer-Schrama SM (2013) Cognitive development in congenital hypothyroidism: is overtreatment a greater threat than under treatment? J Clin Endocrinol Metab 98: 4499-4506.
- Delahunty C, Falconer S, Hume R, Jackson L, Midgley P, et al. (2010) Levels of neonatal thyroid hormone in preterm infants and neurodevelopmental outcome at 5 1/2 years: millennium cohort study. J Clin Endocrinol Metab 95: 4898-4908.
- Wassner AJ, Brown RS (2013) Hypothyroidism in the newborn period. Curr Opin Endocrinol Diabetes Obes 20: 449-454.
- Olivieri A, Corbetta C, Weber G, Vigone MC, Fazzini C, et al. (2013) Congenital hypothyroidism due to defects of thyroid development and mild increase of TSH at screening: data from the Italian National Registry of infants with congenital hypothyroidism. J Clin Endocrinol Metab 98: 1403-1408.
- Rabbiosi S, Vigone MC, Cortinovis F, Zamproni I, Fugazzola L, et al. (2013) Congenital hypothyroidism with eutopic thyroid gland: analysis of clinical and biochemical features at diagnosis and after re-evaluation. J Clin Endocrinol Metab 98:1395-1402.
- Xuesong Cen, Dongmei Cen, Aimin Zhang (2013) Children with congenital hypothyroidism Clinical analysis of rehabilitation training 16: 2901-2903.
- Bargagna S, Astrea G, Perelli V (2006) Neuropsychiatric outcome in patients with congenital hypothyroidism precautiously treated: Risk factors analysis in a group of patients from Tuscany. Minerva Pediatr 58: 279-287.
- Calaciura F1, Motta RM, Miscio G, Fichera G, Leonardi D, et al. (2002) Subclinical hypothyroidism in early childhood: a frequent outcome of transient neonatal hyperthyrotropinemia. J Clin Endocrinol Metab 87: 3209-3214.
 ,
Jianping Chen1, Juan Liu1,Ting Li2 and Fangting Liu1
,
Jianping Chen1, Juan Liu1,Ting Li2 and Fangting Liu1